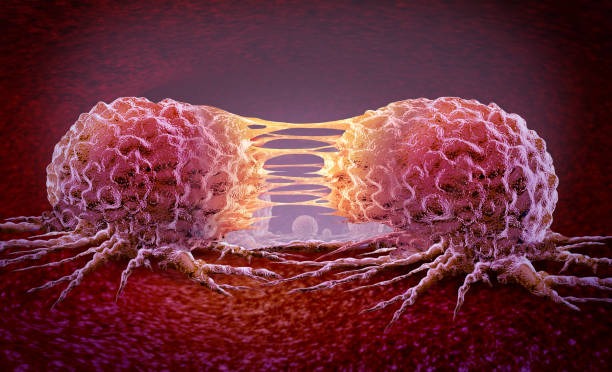
Cancer traditionally was considered a collection of rapidly dividing cells. But in so doing, that simplification does not take into consideration the complicated ecosystem of cells surrounding the tumor, the tumor microenvironment (TME). The TME is not background; it takes an active role in cancer development, metastasis, immune evasion, and drug resistance. Observing how the tumor microenvironment directs cancer growth presents new opportunities for targeted therapy and personalized medicine.
What do you understand about the Tumor Microenvironment?
The tumor microenvironment is known as the cellular and non-cellular environment of a tumor. It includes:
Non-cellular components: Extracellular matrix (ECM), signaling molecules (cytokines, growth factors), oxygen tension, and pH gradient
Blood vessels and lymphatics: Providing nutrients and route for metastasis
The interaction between these cells and cancer cells creates a dynamic and protective niche for tumor growth.
How the Tumor Microenvironment Take hold of Cancer Growth
Maintaining Tumor Cell Proliferation
TME facilitates the uncontrolled proliferation of cancer cells by producing growth factors like epidermal growth factor (EGF) and vascular endothelial growth factor (VEGF). The growth factors induce the proliferation of cancer cells and their survival but prevent apoptosis (cell death).
Facilitating Angiogenesis
A developing tumor requires an influx of blood. TME releases pro-angiogenic factors such as VEGF to stimulate the development of new vessels, also referred to as angiogenesis. The new vessels are designed to bring oxygen and nutrients to the tumor but are faulty, creating a leaky and disorganized vasculature that retards drug delivery.
Enabling Immune Evasion
Under normal circumstances, immune cells clear the body of abnormal cells. But in the cancer microenvironment, immune cells are usually reprogrammed or even suppressed. All tumor-associated macrophages (TAMs), regulatory T cells (Tregs), and myeloid-derived suppressor cells (MDSCs) are capable of creating an immunosuppressive microenvironment, allowing the tumor to escape immune surveillance.
Inducing Metastasis
The TME is a permissive setting for metastasis, or the travel of cancer to remote organs. The ECM is remodeled to enable cancer cells to move, and enzymes such as matrix metalloproteinases (MMPs) break down nearby tissue. Cancer-associated fibroblasts lay tracks in the ECM to lead cancer cells to vessels, seeding metastatic journeys.
Facilitating Therapy Resistance
Chemotherapy, radiotherapy, and targeted therapy are less effective because of TME characteristics such as hypoxia (lack of oxygen), acidic pH, and modified drug metabolism. The cancer cells in these niches are able to be dormant, escape the effects of drugs, and subsequently resurface to encourage relapse.
Key Elements of the Tumor Microenvironment
Cancer-Associated Fibroblasts (CAFs)
These induced fibroblasts support cancer growth through the secretion of ECM components, cytokines, and tissue-remodeling enzymes. CAFs can even cause genetic instability in nearby cancer cells.
Immune Cells
While some immune cells target cancer, others (e.g., TAMs and Tregs) can inhibit immunity and enhance tumor survival. The balance between these two opposing forces will determine disease progression.
Extracellular Matrix (ECM)
The ECM contributes to structural integrity as well as serves as a reservoir for signaling molecules. Modulation of the mechanical properties and composition of the ECM can inform the cancer cells to become more aggressive and invasive.
Hypoxia and Metabolic Reprogramming
Tumors are poorly vascularized and hence are hypoxic. It activates the hypoxia-inducible factors (HIFs), which enable the adaptation of cancer cells by changing their metabolism.
Challenges and Opportunities of Tumor Microenvironment in Treatment:
– Challenges to Treatment: The thick ECM and faulty blood vessels may be the hindrance to effective drug delivery.
– Therapeutic Resistance: TME cells may detoxify anticancer drugs or shield cancer cells.
– Limitations of Immunotherapy: Immunomodulatory TME diminishes the efficacy of immune checkpoint blockers and CAR T-cell therapy.
– New Frontiers: Direct targeting of the TME by reforming CAFs, VEGF blockade, or reactivating immune cells is an exciting direction in cancer therapy.
Future Directions
– Personalized TME Profiling: Monitoring the specific microenvironment of every tumor can lead to custom therapies.
– Nanotechnology: Advanced drug delivery systems can target the TME more efficiently.
– Combination Therapies: TME-targeted drug combinations with conventional chemotherapy or immunotherapy might improve the outcome.
– Biomarkers: TME-associated markers might be able to predict therapy response or the aggressiveness of the tumor.
Conclusion:
By sustaining cancer cells, protecting them from immune attack, and inducing drug resistance, the TME heavily influences the course of disease. Learning more about this microenvironment unleashes the potential for new treatments beyond just killing cancer cells and instead reorganizing the entire tumor environment for improved patient benefit.
FAQs
1. What is the tumor microenvironment, and why is it so important in cancer?
The tumor microenvironment refers to the nurturing cells, molecules, and tissue that fuel and control cancer growth. It is importantly involved in tumor development, immune suppression, metastasis, and drug resistance.
2. How does the tumor microenvironment influence cancer therapy?
It can interfere with treatment through the generation of physical barriers, drug resistance, and suppression of immune responses. These are some of the reasons why it is a useful target in contemporary cancer therapy.
3. Can the tumor microenvironment be targeted by cancer therapies?
Yes. New therapies seek to disrupt the TME, including angiogenesis inhibitors, checkpoint blockade immunotherapies, and agents modifying the ECM or CAFs to enhance outcomes.
4. How does tumor microenvironment hypoxia affect cancer development?
Hypoxia causes cancer cells to evolve by gene expression and metabolic alterations, making them more malignant and therapy-resistant.
5. What is the role of immune cells?
Some immune cells combat cancer, while others become reprogrammed to support tumor growth through suppressive immune modulation and induction of inflammation.